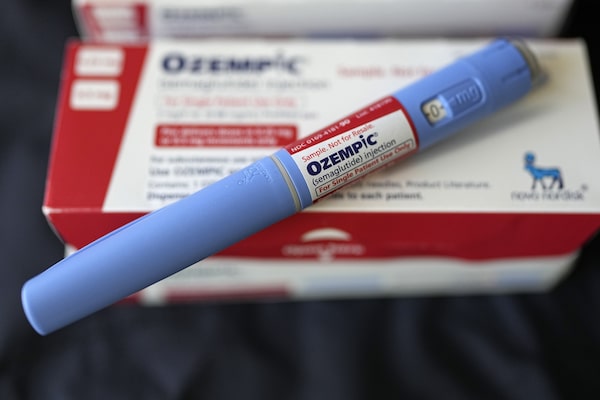
Ozempic, which was designed for Type 2 diabetes but is prescribed off-label in Canada for obesity, works by reducing cravings and making people feel full more rapidly.David J. Phillip/The Associated Press
Ozempic is part of a new class of drugs that many doctors and advocates believe represents the future of obesity treatment. The medication, which was designed for Type 2 diabetes but is prescribed off-label for obesity, works by reducing cravings and making people feel full more rapidly. Although semaglutide – Ozempic’s active ingredient – is not the first drug of its kind to hit the market, scientists believe it appears to work better for weight loss than previous iterations.
In the past year, Ozempic and other semaglutide medications have exploded in popularity, driven by social media and celebrity endorsements. As a result, the drug is in short supply in Canada, with manufacturer Novo Nordisk expecting the shortage to last until March.
Here is an overview of how Ozempic works, other semaglutide medications and what insurance coverage looks like in Canada.
What is Ozempic and how does it work?
First off, Ozempic is the brand name of a Type 2 diabetes medication manufactured by Novo Nordisk. The pharmaceutical company also makes the drug Wegovy, which is specifically designed to treat obesity.
Both Ozempic and Wegovy have the active ingredient semaglutide, which mimics the body’s own GLP-1 hormone that’s produced when there’s food in the intestines. In people with diabetes, this hormone helps the body produce insulin more efficiently. For weight management, it helps people feel a sense of fullness.
“In a nutshell, Ozempic works not by boosting metabolism or melting fat. It works by decreasing caloric intake because people have decreased hunger, decreased cravings and feel full more rapidly,” says Dr. Yoni Freedhoff, a physician and the medical director of the Bariatric Medical Institute in Ottawa.
In an Ozempic clinical trial, people taking the drug lost an average of 15 per cent of their body weight over a 68-week period – when combined with therapy, calorie reductions and other lifestyle interventions. Participants who took a placebo and received the same lifestyle interventions lost only 3 per cent of their body weight. Another study found that people taking Wegovy lost a similar amount of weight over a 68-week period, results that surpass any previous obesity drugs.
Both drugs are administered through weekly injections.
Ozempic and Wegovy are designed to treat chronic health conditions – Type 2 diabetes and obesity – which means the medication needs to be used long term, explains Dr. Freedhoff. In fact, a 2022 study found that most people taking semaglutide gained much of the weight back within a year of stopping the medication.
Who qualifies for Ozempic in Canada?
Health Canada approved Ozempic in 2018 and Wegovy in 2021, but the latter is not yet available here due to overwhelming demand in the United States and other countries. As a result, some doctors prescribe Ozempic “off-label” to treat obesity.
Ozempic must be prescribed by a licensed healthcare professional, such as a family doctor or physician, nurse practitioner or through telemedicine. To qualify for Ozempic, patients generally need to have a body mass index of 30 or above, or a BMI of 27 to 30 with a weight-related medical condition, such as high blood pressure or Type 2 diabetes.
What are the side effects of Ozempic?
Common side effects of Ozempic include nausea, vomiting, diarrhea, stomach pain and constipation. More serious but rare side effects include changes in vision, kidney problems, severely low blood pressure, pancreatitis or severe allergic reactions.
In a study from the University of British Columbia, researchers found that people using Ozempic for weight loss are at a higher risk of gastrointestinal conditions, such as pancreatitis, bowel obstruction and stomach paralysis, compared to those who use bupropion-naltrexone, another medication approved specifically for obesity management. Compared to that other weight-loss pill, which is sold under the brand name Contrave, semaglutide was linked to more than four times the risk of bowel obstruction, which prevents food from passing through the small or large intestine, resulting in symptoms such as nausea and vomiting, the study found.
In September, 2023, the U.S. Food and Drug Administration announced Ozempic’s warning label would be updated to say it may be linked to a life-threatening intestinal blockage. The condition, called ileus, can lead to reduced blood flow to organs. There is no warning about ileus on the Canadian boxes.
Dr. Freedhoff says Ozempic is a very well-tolerated medication. “Having prescribed this medication at least 1,000 times, I’ve probably had to stop it in 2 per cent of patients for side effects. And the only side effects I’ve ever had to stop it for is nausea that’s persistent,” he says. “But if you start the drug at a low dose and you advance it slowly, the vast majority of people see the nausea disappear.”
What are some other concerns about Ozempic?
Some eating disorder specialists believe that Ozempic is contributing to harmful diet culture and weight shaming. The widespread promotion of the drug, including on TV ads, streetcar wraps, sports games and social media, reinforces the idea that weight loss should always be the end goal.
Ozempic promotion is “just another example of how diet culture is telling us that we should lose weight if we can because living in a larger body is a bad thing. And that’s what keeps us in a cycle of diet culture,” said Debra Wells-Hopey, a program manager for Eating Disorders Nova Scotia, in an interview with the Canadian Press.
What other weight loss medications are available in Canada?
Since Ozempic came onto the market, other semaglutide medications have also become available.
Rybelsus
Novo Nordisk, the manufacturer of Ozempic and Wegovy, also produces Rybelsus, which is the pill form of semaglutide. Rybelsus is currently approved by Health Canada for Type 2 diabetes, but is prescribed off-label for obesity.
Tirzepatide
Sold under the brand name Mounjaro, Health Canada approved the Type 2 diabetes medication tirzepatide in November, 2022. Like Ozempic and Wegovy, tirzepatide imitates the GLP-1 hormone, but it also targets a second hormone, called glucose-dependent insulinotropic polypeptide, or GIP. Manufacturer Eli Lilly also sells the drug specifically for weight management under the name Zepbound, but that has not yet been approved in Canada. As a result, some doctors prescribe Mounjaro off-label for obesity.
According to the U.S. Food and Drug Administration, patients who used tirzepatide lost an average of 18 per cent of their body weight when it was taken at its highest dose in a drug trial. In comparison, Wegovy produced an average of 15 per cent weight loss.
A pharmacist displays a box of Mounjaro, a tirzepatide injection drug used for treating Type 2 diabetes.GEORGE FREY/Reuters
Why is there an Ozempic shortage in Canada?
Ozempic is facing a worldwide shortage owing to high demand that’s outpacing Novo Nordisk’s manufacturing capabilities. While the shortage of 1 mg Ozempic pens was resolved in Canada in early January, Novo Nordisk is expecting a shortage of its 0.25/0.5 mg pens until March. “We have taken immediate steps to increase our production capabilities to meet increased demand,” said the manufacturer in a statement. “We are running operations 24/7, building new lines and facilities, and procuring and building new capacity and plants.”
Eli Lilly, which produces Mounjaro (tirzepatide), is also expecting shortages of the drug throughout early 2024.
As a result, Health Canada said that Ozempic and Mounjaro should be conserved for people who have no other treatment options and advised pharmacists to not start new patients on these drugs.
In Europe, lawmakers have set harder restrictions. Belgium issued a new law in November banning doctors from prescribing Ozempic and other GLP-1 drugs for weight loss unless a patient’s BMI is 35 or above and has one underlying health condition. Last summer, in July, Britain called for physicians to only prescribe Ozempic and other GLP-1 drugs for Type 2 diabetes, not for weight loss. Germany is debating banning the export of the medication.
Last April, British Columbia began restricting the sale of Ozempic to people who live in Canada after a huge surge in individuals outside the country filling prescriptions. From Jan. 1 to April 10, around 30,700 Ozempic prescriptions were dispensed from B.C. pharmacies to people with U.S. addresses. (Price was the driving factor behind Americans purchasing Ozempic online in B.C.: a month’s supply of Ozempic in B.C. costs roughly $300. The price in the U.S. can be three times higher.)
The shortage has prompted some medical groups and professionals to call for a moratorium on prescribing the drug for obesity, suggesting that people with Type 2 diabetes get priority access.
But according to physicians who treat obesity, the implied suggestion here is that people with diabetes are more deserving of priority access to semaglutide while it’s in shortage, demonstrating another example of weight bias.
Dr. Freedhoff says that obesity needs to be seen as a chronic health condition, like high blood pressure, and treated accordingly. “The only reason we seem to be upset as a society about the long term use of these medications is weight bias. If this was simply a choice that people could make, people would have made them,” he says.
“There are lifestyle levers that can help some people with high blood pressure – people can exercise more, eat differently, lower their sodium content, sleep and meditate. But we don’t moralize about the people who either don’t want to do those things or don’t see success with those things. We put people on medications to treat high blood pressure because we know that high blood pressure carries with it long term risks.”
How much does Ozempic cost? Is it covered by insurance?
Out of pocket, Ozempic costs around $300 a month in Canada, depending on the pharmacy. If you’re taking the medication for Type 2 diabetes, typically private insurance will cover the costs, as will some provincial/territorial plans if you meet certain criteria.
If you’re planning to use Ozempic for weight loss, it’s best to speak with your provider, since some companies like Manulife do not cover the drug for obesity.
Dr. Freedhoff says, however, that he believes in the future Ozempic and similar drugs will be covered more broadly for weight loss as the benefits of these drugs become clear.
“The benefits are not just risk reduction for common comorbid conditions, like diabetes and high blood pressure, but also likely the most common human cancers,” he says. “Those risk reductions and improved quality of life would affect things like presenteeism, absenteeism and use of the health care system. I think over time, we will without a shadow of doubt recognize that there are real cost benefits to the coverage of these medications.”
With reports from Carly Weeks, The Canadian Press and Reuters